-
Ganesh Talkies, Kolkata
Ganesh Talkies, Kolkata

Preparing for Hysteroscopic Polypectomy properly ensures a smooth procedure and faster recovery. Follow these essential do’s and don’ts for the best experience.
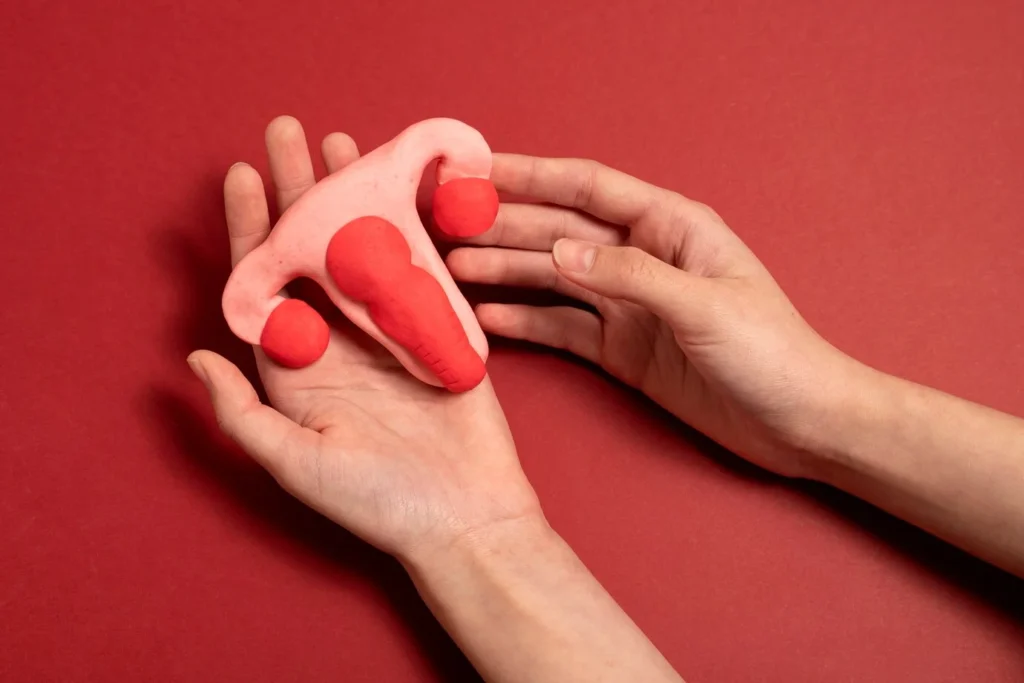
Hysteroscopic polypectomy is a minimally invasive procedure used to remove uterine polyps, which are small, non-cancerous growths in the uterus. These polyps can cause irregular menstrual bleeding, discomfort, and fertility issues. While the procedure itself is quick and safe, preparing for hysteroscopic polypectomy plays a crucial role in ensuring the best possible results.
Proper preparation helps:
If you’re scheduled for this procedure, you may have many questions, such as:
In this guide, we’ll cover the essential do’s and don’ts of preparing for hysteroscopic polypectomy, ensuring that you are well informed and confident before your procedure.

Hysteroscopic polypectomy is a surgical procedure performed using a hysteroscope—a thin, lighted tube inserted into the uterus through the vagina. This allows the doctor to remove polyps without making any external incisions.
This procedure is recommended to:
Since it is a minimally invasive procedure, recovery is usually quick, and most women return home the same day. However, preparing for hysteroscopic polypectomy correctly can make a significant difference in your overall experience.
Your gynecologist will provide specific pre-surgery instructions based on your medical history. These may include:
Blood Tests and Imaging – Routine tests to check your overall health.
Stopping Certain Medications – Blood thinners and anti-inflammatory drugs may need to be discontinued.
Allergy and Medical History Review – Inform your doctor about any allergies or existing conditions.
Good nutrition helps in faster recovery. In the days leading up to the procedure:
Eat light, easily digestible meals to prevent bloating.
Increase fiber intake to avoid constipation post-surgery.
Stay hydrated by drinking plenty of water.
Avoid excess caffeine or sugary foods, as they may cause bloating.
Most doctors recommend fasting for at least 6-8 hours before surgery if general anesthesia is used. This helps prevent complications like nausea or vomiting during the procedure.
Since you may feel drowsy or weak after surgery, arrange for a friend or family member to drive you home. Having someone to assist you for the first 24 hours is recommended.
On the day of the procedure:
Choose loose, comfortable clothing to wear to the hospital.
Avoid tight pants or dresses that may cause discomfort after surgery.
Do not use tampons, douches, or vaginal creams for at least 24-48 hours before the procedure. These may interfere with the surgery.
Avoid sexual intercourse for a day or two before surgery, as irritation may affect the uterine lining.
Smoking and alcohol can slow down healing and increase the risk of complications. Try to avoid them for at least a week before and after surgery.
Do not take aspirin, ibuprofen, or other painkillers unless prescribed by your doctor. These medications can increase bleeding risk.
If you experience fever, flu-like symptoms, or unexpected vaginal bleeding before the procedure, contact your doctor immediately.
After the procedure, you may experience mild cramping, light spotting, or drowsiness, which is normal.
Rest adequately – Avoid strenuous activities for a day or two.
Eat light meals – Stick to a soft diet if you feel nauseous after anesthesia.
Take prescribed medications – Follow your doctor’s instructions carefully.
Stay hydrated – Drink plenty of water to help your body heal faster.
Follow up with your doctor – Attend any scheduled post-op check-ups.
Avoid heavy lifting or intense exercise for a week.
Do not engage in sexual activity for at least a week.
Avoid public pools, hot tubs, or swimming to prevent infection.

You should follow fasting instructions, wear comfortable clothing, and arrange for someone to drive you home. Avoid using vaginal products or taking unapproved medications.
Most doctors recommend fasting for at least 6-8 hours before surgery, especially if general anesthesia is used.
No, it is a minimally invasive outpatient procedure, and most women return home the same day.
Most women can resume light activities within 1-2 days, but heavy physical work should be avoided for at least a week.
Mild spotting is normal, but if you have excessive bleeding, severe pain, or fever, contact your gynecologist immediately.
Preparing for hysteroscopic polypectomy properly ensures a safe, stress-free experience and a quick recovery. By following essential do’s—such as fasting, arranging transportation, and avoiding certain medications—you can minimize risks and enhance surgical success.
If you have concerns, please don’t hesitate to ask a trusted gynecologist for expert guidance. The right preparation will not only make your procedure smoother but also lead to a healthier and more comfortable recovery.